What is the vaginal microbiota?
The vaginal microbiota consists of 90% lactic acid bacteria (lactobacilli) which colonise the vagina at puberty and form what is known as the Doderlein flora (named after the gynaecologist Alfred Döderlein who first described it in 1892). The vaginal microbiota also consists of other bacteria such as Gardnerella vaginalis, Atopobium vaginae and Prevotella spp, as well as fungi such as Candida albicans, and it is overgrowth of these that can cause infections.
The essential role of lactobacilli
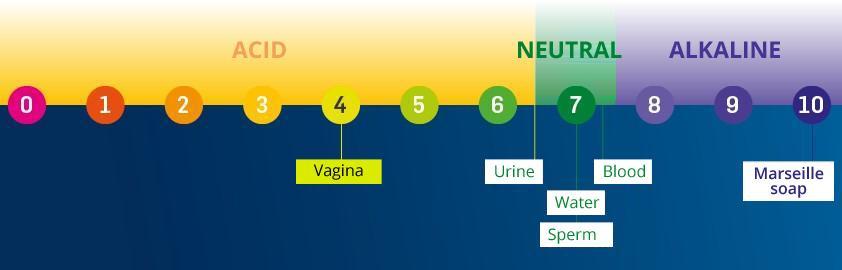
Lactobacilli have very specific functions. They stimulate the local immune system and form biofilms which create a protective shield over the vaginal wall. They convert the glycogen secreted by genital mucosa cells into lactic acid, thus creating an acid environment which is needed to keep the vaginal pH between 3.5 and 4.5.
The vaginal pH reflects the state of the vaginal microbiota; a pH above 4.5 indicates that there is an imbalance in the vaginal flora, also known as dysbiosis. When dysbiosis is accompanied by symptoms such as unusual bleeding or vulval pain or itching, an infection can occur and must be identified and correctly treated. The pH during the menopause is naturally 4.5.
Every woman harbours several types of lactobacilli which will change during her cycle and during her lifetime according to hormonal variations, her environment, her intimate hygiene, her sex life, etc.
The composition of the flora can therefore be as follows:
- Dominated by Lactobacillus crispatus (48% of women)
- Dominated by Lactobacillus gasseri (23.5% of women)
- Dominated by Lactobacillus iners (20% of women) – slight flora imbalance
- Dominated by Gardnerella vaginalis (total flora imbalance - 30% of infections)
- Dominated by Lactobacillus jensenii (25% of women)
In women with dysbiosis, providing good bacteria in the form of probiotics could have a favourable effect on the vaginal microbiota. Lactobacillus crispatus, L. gasseri, L. rhamnosus and L. plantarum have antiviral and antibacterial properties and will help to inhibit the growth of pathogens, limit their expansion and prevent pathogen biofilm formation.
Vaginal microbiota that evolves throughout life
Lactobacilli are entirely dependent on oestrogen impregnation, i.e. on the secretion of oestrogens, female sex hormones produced mainly by the ovaries.
A woman’s vaginal microbiota therefore changes throughout her life according to her hormonal status:
- The vaginal flora is created at puberty. Oestrogens will thicken the vaginal mucosa and allow glycogen to be produced. Rectal lactobacilli will then be attracted to and colonise this new favourable environment.
- During a woman’s period, the alkaline pH of the blood increases the vaginal pH. Lactobacilli decrease, leaving more room for pathogens.
- A woman who is pregnant produces more hormones (HCG, oestrogens, progesterone, oxytocin, etc.) which cause an increase in lactobacilli. The more oestrogen is produced, the more vaginal cells release glycogen, which serves as an energy source for lactobacilli but also for Candida albicans. This is why pregnant women are more prone to fungal infections.
- At menopause, there is a progressive reduction in oestrogens and therefore in lactobacilli, varying widely between women. The menopause is accompanied by vaginal dryness in 55 to 70% of women*. A preventive course of probiotics could restore the balance of the flora and limit the appearance of infections.
Dysbiosis can become established due to these hormonal variations, but also to lifestyle (tobacco use, medications, antibiotics, stress, etc.), and cause vaginal disorders such as fungal or vaginal infections or cystitis. In addition to a healthy lifestyle, probiotics and plants such as orthosiphon, pilosella or cranberry can be used preventively to help maintain the balance of the vaginal microbiota and avoid recurrent fungal and urinary-tract infections.
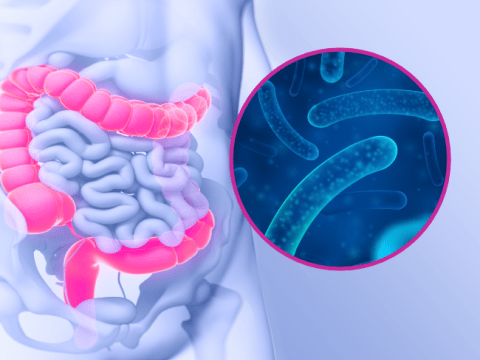
A close link between vaginal microbiota and gut microbiota
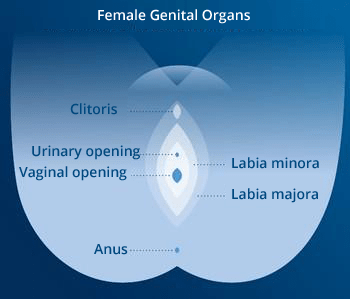
The natural reservoir for vaginal lactobacilli is the gut. Bacteria pass from the anus to the vagina across the perineum and vulva via the hydrolipidic film which covers the skin surface. So the vaginal microbiota “inherits” some of its bacteria from the gut microbiota.
For example, Candida albicans involved in yeast infections is also present in the gut microbiota. It can be present in a latent form throughout the host’s lifetime. Candida overgrowth is triggered by a reduction in immune defences, an imbalance in microbiota and/or the influence of predisposing factors such as hygiene, the hormone cycle or stress.
For this reason, it is important to preserve or restore the balance of not only the vaginal microbiota but also the gut microbiota, as they are closely linked.
The vaginal microbiota therefore consists of numerous essential bacteria for good vaginal health. Solutions such as probiotics or certain plants, combined with a healthy lifestyle, can help restore or preserve the best balance for healthy vaginal microbiota.